
Kako bismo Vam što više približili problematiku umjetnog kuka, pokušat ćemo odgovoriti na nekoliko najčešćih pitanja pacijenata.
During years of experience in working and talking to patients, we can conclude that there are two groups of patients:
- Larger gorup – group that wants to know „everything“ about their disease, browsing the websites, asking friends, consulting patients who had or have similar problems and finaly ask for the second opinion
- Smaller gorup – group that suppresses the disease, dosen’t want to know anything about it and blindly leaves themself to doctor’s knowledge and lidership
It si not our intention to forse any of the groups here because, as always, each has its pros and cons, but, if you belong to the second group, you probably haven’t read this at all and if you did, now is the time to move to the happier topics. If you belong to the first group, here we will introduce you to the basics of your hip disease (or trauma) and basic features of hip replacement therapy. Often patients come for the examination by the operator with prepared questions they want to ask, which is certainly necessary, but, in order not to forget the most important thing you want to know, we are trying to help you and we will try to answer to few of the most frequently asked questions.
The hip joint is a complex network of bones, cartilage, muscles, ligaments and tendons that have to work as one unit. It is one of the most used joints in the human body and allows us to walk, sit, bend and turn the legs without pain.
Hip joint is very stable joint, which is composed of the spherical part (femoral head) at the top of the femur, which enters to the concave articular part, a socket, which consists of the pelvic bone. Both articular parts are connected by ligaments, which form the joint capsule, and together with the position of bone fragments, are responsible for the stability of the joint.
Articulating parts, head and cup, are coated with layer of smooth tissue called cartilage. The capsule surrounds the joint secreting the fluid (synovial fluid). This fluid lubricates the joint, further reducing friction and facilitating movement.
Injury or disease can cause damage to the hip joint in several ways: damage bones (fractures) or wear out the cartilage (degenerative diseases). The most common causes of pain in the hip are: osteoarthritis (OA, rheumatoid arthritis, osteoporosis, osteonecrosis (death of bone caused by insufficient blood supply), injuries, infections, and bone tumors.
Coxarthrosis is one of the most common diseases of the hip in the elderly. It is characterized by the gradual development of degenerative changes in articular cartilage and later the in other joint structures. The most common primary factors are older age, congenital developmental anomalies of the hip joint, being overweight, traumatic damages, inflammations, local circulatory disorders and others.
Symptoms that indicate hip damage are:
1. Pain At first, fatigue occurs and occasional soreness at higher loading of the affected joint, pain after long periods of stagnation and pain when descending the stairs and later experiencing pain during rest, as well. The patient wakes up at night because of the pain, requiring the use of analgesics (painkillers). It occurs most often in the groin, gluteal area, and in the knee, also.
2. Contracture (stiffness) At first, transient numbness in the first movement and a limited range of particular motions (mostly internal rotation) appears. Later, the stiffness becomes fixed, and stiffness of rotatory movement is particularly evident.
3. Leg shortening The shortening of the legs is the result of wear of the cartilage on the head of a thigh bone and in the area of the socket, and deformation of thigh bone head and its displacement upwards (cranially).
4. External rotation of leg– a result the stiffness of leg at hip
5. Limp
6. Muscle atrophy
- Medical history
- The patient describes his difficulties, pain during movement and / or at rest, night pain, taking pain medications (temporarily or permanently)Mobility – limping while walking, walking with a cane, one or both
- Clinical examination
- your doctor will examine in detail the mobility of your hip, numbness, loss of muscle length and muscle volume of the leg.
- X-ray
- X-ray image will reveal the cartilage loss and changes in the head of a thigh bone and the joint socket. It is useful to make a recording and lumbar spine, because signs of the disease can often be mixed.
- MRI
- rarely used to detect early stages of disease
- Other diagnostic methods
- are not implemented as standard but only upon request from your doctor
In case of injury (hip fracture), your doctor will determine the type of surgery, and for certain hip fracture, complete (TEP) or partial (PEP) hip replacements will be an ideal solution, and the surgery should not be delayed.
In hip diseases, as well as in almost all diseases, there is a conservative and operational treatment.
Conservative therapy, painkillers (analgesics), and various physical therapy treatments can reduce pain and improve mobility in the hip, but can not directly affect the cause of the disease.
Pain and mobility of the patient decide on the time of the operation and, when they become unacceptable, it is necessary to opt for surgery.
The progress of medicine and technology has turned the hip replacement in one of the most successful procedures, with very long survival period and therefore, in consultation with a doctor, one should opt for the surgery at a time when disturbances disrupt everyday life.
In some cases, your doctor can advise you on the earlier decision for the procedure to avoid further damage to the articular parts of the hip, because delaying the surgery would make it less successful.
Many hip diseases, whether inflammatory or degenerative, affect both the articular parts, socket and the head of thigh bone. Articular cartilage on both articular parts is damaged and gradually disappears. When walking and moving, bone to bone friction appears and causes pain. At a later stage, changes in the bones of the pelvis and the head of the upper leg appear. In some diseases (aseptic necrosis of the head of the upper leg) and injury of upper part of a thigh bone, the damage is related only to the head of a thigh bone. Type of surgery depends on the damage and on the age of the patient.
Total hip endoprosthesis (THE) – Represents the complete replacement of two articular parts, pelvis socket and thigh bone head. After removing the head and neck portion of a thigh bone, and cleaning pelvis socket, both articular parts are replace with implants, and thus creating a new hip joint.
Cover (resurfacing) prostheses – Only the damaged part of the joint is replaced, such as the articular surfaces, and the metal cup is placed on the treated head of the thigh bone, without cutting, and in articula socket a metal insert – cup is placed.
Partial hip endoprosthesis (PHE) – Represents partial replacement of only the femoral part of the joint (upper thigh bone). This type of prostheses is performed mainly in fractures of the neck of a thigh bone in elderly.
All these types of prostheses can be cementless and cement, depending on the way in which are fixed in the bone. In cementless prostheses, a metal implant is fixed directly to the bone so that the implant, which is usually 1 mm oversized compared to the treated implant position, is pressed into created dent. On the surface of the metal implant there are small filisters for bone ingrowth. In cemented prosthesis, bone cement is inserted between the bone and the implant to bind them together.
DESCRIPTION OF OPERATING PROCEDURE Here are the principles of surgical treatment, which are always adopted to the characteristics of the individual patient.
The night before the operation you will get an injection into the subcutaneous tissue of the abdomen. The injection of anticoagulant, thus reducing the risk of thrombosis. The risk of infection can be reduced by antibiotics, which you will receive shortly before the surgery.
On the day of surgery, before going into the operating room, you will receive a sedative, which will allow your calm induction of anesthesia. Anesthesia is deliberately provoked loss of sensation, especially pain, in order to perform the surgery. After anesthesia performs, you are positioned on the operating table. Position of the patient on the operating table can be either in the back or side. Both approaches are described and applied in practice and do not differ in the final outcome. Then, in order to achieve sterile conditions in the operating procedure, operation site is preoperatively washed, using special disinfectants, and covered with sterile blanket. Electrodes which allows an use of electrical device (knife, coagulator, etc.) during surgery are cleaved to your body.
Surgery itself starts by cutting the skin and subcutaneous tissue on the side of the hip. After cutting and distracting of soft tissue, we come to the hip joint capsule, depending on the surgical approach. The following is the opening of the joint – arthrotomy, and dislocation of femoral head from the pelvic socket. Osteotomy is performed at the correct angle (cutting femoral neck) in order to process the place for femoral component of the artificial joint. Damaged articular surface of the pelvis socket is treated with special instrument set in order to enable insertion of artificial joint cup. Likewise, the processing of the femoral (thigh) part is done.
When both provisionally parts of hip replacement are temporarily placed, after controlling conformity of the joints, measuring range of motion and limb length, and, finally, testing the stability of artificial joint, installation of the original parts follows. In cases where we have an under-developed pelvis cup or when we have a loose bone or insufficiently stable artificial joint cup in the processed insertion site, cup can be additionally secured with screws. We may also use your own (autologous) or someone else’s (donor) bone to upgrade the existing (noticed) defects. If autologous vascularized graft is used, additional incision in the lower abdomen is made in order to prepare vessels and separate the vascularized graft from the wing of the iliac bone, and then transfere it to the a joint cup where is additionally fixed with screws. If necessary, the wing of iliac bone is further fixed with screws, also. Next is the closure of the operating site in layers applying resorbable sutures, with placing one or two tubes – drains to control postoperative bleeding. The skin is sewn with leather, nonabsorbable sutures, or a set of metal clasps is used. Operation ends by placing sterile gauzeon the wound, and elastic bandage over the entire leg. Finally, the radiological record i smade in order to confirm the good position of the implanted components of the endoprosthesis. After the surgery, patient is transferred to the department or, upon the dicision of the anesthesiologist, to the intensive care unit. The patient stays at the department for 5 – 10 days, during which initial physical therapy takes place.
Femoral component of the cement and cementless hip prosthesis is modular and consists of the head and body (stem). The head is made of cobalt and chromium alloy, while the body is made of titanium alloy.
Joint cup in cement prosthesis is made of polyethylene, and in cementless prosthesis there are acetabular metal cup made of titanium alloy and polyethylene liner.
The most common complication of hip replacement is deep vein thrombosis (blockage of the venous system of the leg by a blood clot), and much less common pulmonary embolism (blockage of a lung artery by a blood clot). To reduce the possibility of embolism, prophylaxis is regularly carried out, including:
- Anticoagulant therapy (medications that prevent the formation of blood clots)
- Wearing elastic stockings during and after the surgery.
- Early patient mobility
Anticoagulation therapy starts before surgery (depending on the protocol of each hospital) by receiving the drug into a vein, and it is in this form applied during hospital stay. Intravenous drug can be applied during the entire time, but most often the drug is replaced with a drug that is taken by mouth. During the usage of any of these drugs, it is necessary to regularly control the “dilution of blood” in order to be keep therapy effective and avoid unwanted bleeding.
Today there are new anticoagulant drugs in which blood tests are not necessary.
Anticoagulation therapy is applied to the full mobility of the patient, and at least 1 month after surgery.
Wearing elastic stockings is important tromboprophylaxic measure and stickings must be worn on both feet.
Details of anticoagulant therapy should be discussed with your doctor.
In order to make surgery painless and as pleasant as possible for the patient, the THA is, like all surgical procedures, performed under anesthesia. In the past, the most common form of anesthesia was general endotracheal anesthesia, where the patient is asleep during the surgery, and the doctor anesthesiologist completely controlls his vital functions.
With the development of medicine, the risks of general anesthesia are reduced by the introduction of local anesthesia, where the patient at surgery control its vital functions himself, and oerating part of the body is painless. Today, the majority of hip prosthesis is performed in this type of anesthesia, but the type of anesthesia is decided by the anesthesiologist in consultation with the patient.
ASSOCIATED RISKS:
Implantation of hip replacement is the big, but routine, orthopedic surgery. However, like all other surgical procedures, the procedure can be accompanied with certain complications / problems, also. We will mention those that occur more frequently in hip arthroplasty procedure. Some risks may be higher or lower, depending on the type of surgery, the extent of damage to your hip, as well as other diseases that you may suffer. However, it is extremely important that you have realistic expectations about your surgery and its outcome from the beginning.
COMMON COMPLICATIONS:
1. Blood loss during and immediately after surgery – For large areas of spongy bone that is being exposed during surgery, serious bleeding that would require transfusions and blood products can be caused. Although the blood components, as well as bone grafts, are tested for blood transmissible deseases, there is no 100% guarantee that you can not be infected with HIV, hepatitis, Jakob Creuzfeldt or another, blood transmissible, disease.
2. Thigh bone and / or pelvis fracture during and after surgery – Occur more often in patients with “soft bones” (eg. in patients with rheumatoid arthritis), in overweight patients, patients who have had surgical procedures in the hip, etc.
3. Damage or injury to the surrounding muscles or tendons – Occurs rarely, but may result in reduced function of the hip.
4. Blood vessels injuries – Large blood vessels (arteries and veins) in legs are rarely injured (0.1%). If there is a significant injury of the great vessels, which are located in the front of the hip, it can result in amputation of the leg and, in exceptional cases, even fatalities. However, this happens very rarely. When preparing autologous bone graft, risk of injury to major blood vessels of the pelvis is increased.
5. Nerve injury – Complete or partial injury of large leg nerves are rare (1 to 2%), but serious complications result in full or partial recovery, or recovery of injured nerve never occurs. Damage of n. iatrogenic sciatic nerve occurs in up to 5 – 6% of patients who had a developmental disorder of the hip which caused the functional extension of the extremities, and formed nerve stretching (can be stretched from 3 to 5 cm without neurological disturbances). When using vascularized graft, outbursts of n.femoralis, n.cutaneus femoris lateralis and other nerves close to the hip may also occur.
6. Instruments breakage – Instruments used during surgery can break inside your hip. It is a rare complication. If it happens, broken piece can almost always be removed without consequences.
7. Poor effect of bone cement – It can lead to a number of both local (damages of neurovascular structures, tendons, muscles, quadriceps, bladder, intestines, or other organs, as well as free intraarticular body within the acetabulum) and system complications (general interference in the polymerization, drop in blood pressure, heart arrest, dermatitis).
8. Compartment syndrome – a rare complication that occurs when pressure within the muscle compartments (sections) of thigh and calf becomes greater than the pressure in the blood vessels that supply these sections. This can result in damage to the muscles and neurovascular structures within these sections with all their subsequent consequences.
9. The risks of use of bone grafts from the bone bank – During surgery, need for the use of bone grafts from the bone bank may occur. Their use, as well as the above mentioned use of various blood components, carries the risk of transmission of the aforementioned diseases.
10. Delayed wound healing – It can occur in case of poor local characteristics of the tissues that cover the hip; previous surgical procedures in the area, poor circulation, a large layer of body fat, etc.
11. Skin burns caused by poor electrical contact of electrical knife electrodes – It happens very rarely during surgery.
12. Cutaneous allergic reaction to disinfectant and adhesive tape that secures sterile cloth – It happens very rarely.
13. Postoperative hemorrhage in the hip – It may require subsequent removal of the accumulated blood. Retroperitoneal hemorrhage may occcur as well – hemorrhage in different areas in the abdomen and pelvis and intramural hemorrhage – hemorrhage in the muscle wall.
14. The swelling of the genitals – Rarely occurs and is usually withdrawn in a few days.
15. Periprosthetic heterotopic ossification – Rarely occur after surgery and only 10% affect the range of motion in the hip. In case of significant restrictions of hip movement, sometimes it is necessary to remove them by operating.
16. Difference in the postoperative length between the lower extremities – Occurs in up to 32% of cases, usually as a result of a stable interaction of hip prosthesis components. Usually, after replacement of the other hip, if there is a medical indication for it, leg length is leveled. Rarely, the length difference between extremities causes disorders which require re-operation of the same hip.
17. Postoperative infection – It can occur as superficial (skin) or deep (within the joint) hip infection. Infections after total hip arthroplasty are extremely rare (from the usual 0.3% to 6.2% in men after urethral surgery). Skin infection is usually treated with antibiotics that are taken by mouth (orally). In case of deep infection, it will take a long-term and complex treatment. Prolonged or repeated hospitalizations is necessary during which the hip is accessed again in order to remove the infected tissue. During this procedure, usually infected endoprosthesis is removed as well. The patient receives long-term intravenous, then oral antibiotics. In the case of infection treatment, endoprosthesis can be re-installed, or arthrodesis, hip stiffness, is performed. Extremely rare, septic conditions that require surgery can occur that, beside general procedures, require intensive targeted use of antibiotics. Although rare, there are fatalities caused by infection of hip endoprosthesis described.
18. Phlebitis-phlebothrombosis (blood clots) – Deep vein thrombosis, or blood clots, are a complication that occurs during total hip arthroplasty, as well as in any other surgery on lower body.
19. Pulmonary embolism – If there is a blood clot tear off, it can be carried by blood stream, reach lungs and cause a sudden feeling of shortness of breath, rapid heartbeat, and in rare cases can result in sudden death.
20. Reflex sympathetic dystrophy – This rare disorder is characterized by abnormally prolonged pain of excessive strength.
21. Endoprosthesis dislocation – It occurs in 0-10% of all implanted endoprostheses. When implanting revision endoprosthesis, the risk of dislocation rises up to 20%. Depending on the direction of the hip dislocation, leg is in external or internal rotation, and the patient is able to use functional leg. Depending on the cause / causes of dislocation, it will be decided whether on the conservative or on the operating treatment.
22. Endoprosthesis loosening, wear and / or breakage of prosthesis components – Artificial hip, ie. THA, is complex mechanical device whose individual parts or assemblies do not always function well, ie. can be worn or broken (after 7 years 3% incidence, and after 10 years 25% incidence) and, after a while, it may be necessary to replace some components or complete endoprosthesis.
In total hip arthroplasty also may occur:
1. Bruises – In the area of knee, lower leg or thigh, but they are not considered real complications of this treatment.
2. Painfull scar – Not uncommon. The pain occurs either spontaneously or at the touch of a scar. For the success of the surgery, you are obliged to comply fully all the advice and recommendations from your operator, because it will affect the final result of your surgical treatment.
The first postoperative day starts with exercises on the bed. Avoid placing legs one over the other. Keep legs slightly apart with pillow between legs. If necessary, painkillers are prescripted and anticoagulant therapy is continued. Next is sitting on the bed and getting up with the assistance of a physiotherapist. Avoid sudden rising. Even before the operation it is necessary to have two loftstrand crutches, because you will need them immediately after the surgery. With the help of a physiotherapist you will learn to walk with crutches. The initial load on operated leg is 10 – 15 kg, but it is determined by the operator for each specific case. On the second or third postoperative day the drains are extracted. The patient leaves the hospital between 5 and 10 days after the surgery, unless there are complications, but it also depends on how the rehabilitation is organized or what are the conditions at patient’s home. It is recommended to walk with both crutches for 6 weeks, followed by 3 months of walkind with one crutch. It is important to know that, while walking with one crutch, the one for the opposite leg than the operated is used. Throughout the entire time avoid bending the legs in hip more than 90 degrees, do not place legs one over the other and do not carry any burden.
Today, total hip endoprosthesis is among the most successful surgeries. The success of these operations is extraordinary, and survival * of prostheses extremely high. While in the past the age limit for these surgeries was sought to raise as much as possible, today there is no need to delay indicated surgery because, in this way, patients significantly improve the quality of life when they need it most. For easier insight into the survival of hip prosthesis we will just mention some data from the world literature.
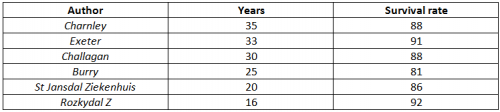
From the above data, we can see that the percentage of survival of prostheses is very high and that by new, particularly cementless prostheses, we can expect the percentage prostheses survival over 95%, which practically means that the prosthesis are in most patients lifelong. However, you should know that, even after complete recovery from hip surgery, there are still some limitations. Normal daily activities are usually completely possible, but some intense sport activities, such as running, basketball, gymnastics, are not recommended. Recommended are walking, golf, swimming, cycling and so on. *Prosthesis survival is prostesis percentage after X years in which new surgical procedure wasn’t necessary.

